Loren Wilson calls having COVID-19 "the flu times two."
Wilson lives in Sun Valley with his wife, Anita, and their two children. It was late October when he first felt a little sick. He started getting a bit of a cough on a Saturday night. It wasn't bad enough to stop him and his family from their usual gathering on a Sunday to watch the Broncos. He remembers someone made nachos.
Then Monday rolled around. He could barely move. He would test positive for the coronavirus about five days later, after staying mostly in bed. Anita and their two daughters ended up testing positive as well. Wilson had more serious symptoms that led him to go to the emergency room about a week after, where he learned his oxygen was very low. Anita ended up hospitalized as well.
"I can get up and walk, but I gotta have this oxygen. It has to be with me," Wilson said, looking toward a 3-foot oxygen tank.
Wilson, 60, is Sioux and was born and raised in Denver. He said his parents moved here from the Sisseton Wahpeton Oyate reservation in South Dakota roughly five years before he was born. He's retired from a career in The Denver Post's printing department.

His case is one of many in a recent spike among Native Americans and Native Alaskan residents in Denver. Census data shows 0.4 percent of Denver residents are Native American, but data from Denver Public Health shows they make up 0.9% percent of all COVID-19 cases as of Dec. 15.
Wilson started feeling symptoms on Oct. 24; he tested positive on Oct. 29. Wilson said he wasn't aware of the spike.

The spike coincided with an increase of cases across the city and across most racial demographics, including white residents in Denver. Overall, the data shows Native American and Native Alaskans have accounted for 0.9 percent of all COVID-19 cases since the start of the pandemic. Hospitalizations have also increased statewide.
Nationwide, the Centers for Disease Control said in August that Native American and Native Alaskans are at higher risk of serious outcomes from COVID-19. And an article from Science magazine noted there have been issues with data collected on Native communities, which makes it harder to figure out the full impact of the pandemic on them.
Wilson got his positive test at the Denver Indian Health and Family Services clinic in Sun Valley.
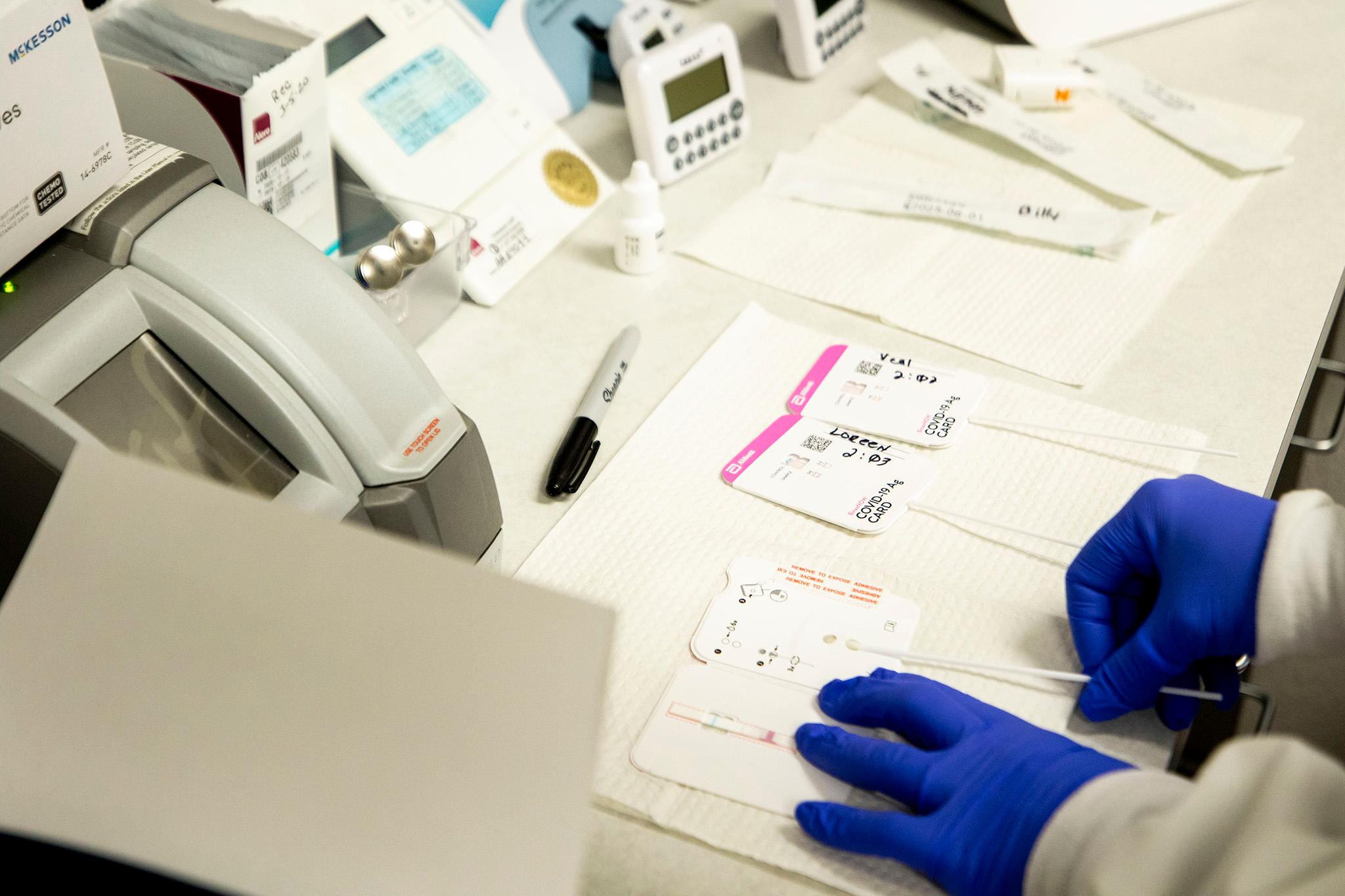
Director of Primary Care at the clinic Karen Hoffman has been monitoring Wilson and his family since then. The clinic provides services including coronavirus testing and behavioral and dental care to Indigenous patients in the metro area.
The clinic is affiliated with the federal Indian Health Service. Hoffman, a nurse practitioner, said most services provided there are free, though patients must prove they have tribal blood or have a tribal card to show their affiliation.

"This is just the rapid one, so it's a little bit inside of each nostril, OK?" Hoffman said as she administered the test to Anita Wilson while she was still inside her car last week. Hoffman then moved to test Lilly Flores Wilson, a 4-year-old sitting in the back seat. "Remember, this is just a little tickle, right, not anything scary."
The Wilsons had stopped by on Nov. 24 to get a follow-up rapid COVID-19 test. Both Wilsons and three other family members tested negative.
Hoffman said the clinic gets patients from the metro area and sometimes from other nearby states or reservations. She said about 70 percent of its patients are from the Front Range. She said the spike in cases among Indigenous in Denver is split between people who are housed and those who are unhoused.
She noted Indigenous people who are experiencing homelessness may use things like public transportation or shelters or services that can lead to COVID-19 exposure.
"Those groups don't have an opportunity to choose when they're going to be quarantined or when they're going to try and isolate themselves," Hoffman said.
Residents who are uninsured or underinsured but who are housed are less likely to seek help until they're very sick, though Hoffman said this is not unique to Indigenous people. However, she added that there are higher rates of hypertension and diabetes among this group, which can lead to additional complications if they get the coronavirus.

"Historically, Native Americans are hesitant to trust medical entities or any entities that they view as part of the government, just because of historical trauma," Hoffman said.
Denver Public Health Director Dr. Bill Burman said the city isn't entirely sure why there's been an uptick in Native populations, but he did note that the cases seem to be tied to areas in Denver that have had high infection rates since the pandemic started. They include southwest and far northeast Denver, areas where the city has not hosted community testing sites.
Anita Wilson thinks her husband's symptoms may have been more treatable if he was able to get to a hospital sooner.
Wilson contacted the family service clinic but was referred to the ER to make sure he would get the necessary treatment.
Both Anita and Loren spent time self-isolating in two different bedrooms when they got sick. Their daughters would cook and leave food outside their doors.
Wilson is still recovering from the virus. He still gets bad headaches and is trying to schedule an appointment with a pulmonologist to make sure there isn't anything serious going on with his lungs.
"I'm stuck with this thing," Wilson said, again looking at the oxygen tank. "It's kind of an inconvenience ... but it just seems so slow, the process here. I guess it affects people in different ways. The way it's affected me is that oxygen will not stay up for anything."

Wilson remains pretty upbeat in recovery. He tried tracing back where he was and what he did before the symptoms started. He blames himself for getting his family members sick.
He has a message for people who don't think COVID-19 poses a threat to them or who think it's a hoax.
"It is real," Wilson said. "Do what they're asking us to do. Wear that mask. It's not that difficult."
Editor's note: Some of the figures in this story were updated after Denver Health notified us it had recorded some data incorrectly.













